- Fri. Apr 19th, 2024
Latest Post
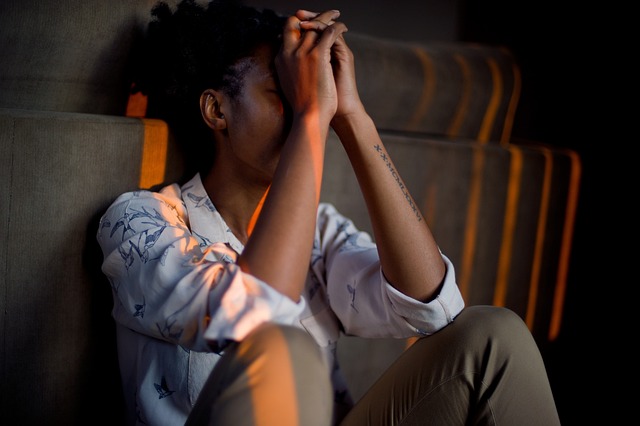
Navigating Stress in Stress Awareness Month 2024: Strategies for a Resilient Mindset
As April unfolds, so does Stress Awareness Month, a timely reminder to pause and reflect on the complexities of modern…
Understanding IBS Awareness Month 2024: Shedding Light on Irritable Bowel Syndrome
Every April, a significant spotlight shines on a condition affecting millions worldwide: Irritable Bowel Syndrome (IBS). IBS Awareness Month, observed…
Mistaken identity vandalism at High Peak Steels premises.
Glossop, Derbyshire based specialist steel stockist High Peak Steels have issued a statement following a recent overnight incident of ‘mistaken…
Enhancing Intimacy: The Role of Sexual Toys in Strengthening Relationships
Enhancing Intimacy: The Role of Sexual Toys in Strengthening Relationships In today’s open society, sexual health has become an integral…
Enhancing Emotional Stability and Well-being
Sexual activity is not merely about fulfilling a physiological need; it is a holistic experience intertwined with emotions, psychology, and…
First-Time Home Buyers: Essential Tips on Choosing Boile
First-Time Home Buyers: Essential Tips on Choosing Boiler Cover Embarking on the journey of homeownership is a monumental milestone, filled…
Where to go for nice walk with the Dog if your away for the Weekend in London?
London is a vibrant city with plenty of parks and green spaces to explore with your furry companion. If you’re…
Where to go for nice walk with the Dog if your away for the Weekend in East Midlands?
Dogs are considered to be man’s best friend and it is important to ensure that they receive enough exercise and…
Where to go for nice walk with the Dog if your away for the Weekend in West Midlands?
List of Places to Visit The West Midlands is a beautiful region with plenty of options for taking your furry…
Where to go for nice walk with the Dog if your away for the Weekend in Wales?
When you’re away for the weekend in Wales and you’re looking for a nice place to take your dog for…
Where to go for nice walk with the Dog if your away for the Weekend in Yorkshire?
List of Where to go for a nice walk with your dog in Yorkshire When you’re away for the weekend…
5 ways insurance is beneficial to your health
Introduction: Life insurance is often regarded as a tool for providing financial protection to loved ones in the event of…
Leveraging Book Printing for Marketing Your Business
Book printing is a powerful tool businesses can use to enhance their marketing efforts. This traditional form of media can…
Where to go for nice walk with the Dog if your away for the Weekend in North West of England?
List of Where to go for nice walk with the Dog if your away for the Weekend in North West…
Why Trusting an SEO Agency In Manchester is Vital in Today’s Digital Landscape
In this digital age, staying ahead of the curve means more than just understanding the basics of SEO—it requires navigating…